If you live outside the US, medical billing sounds simple. You just go to a hospital, get your treatment, and they just bill you. But in the United States, medical billing is one of the most challenging things about running a healthcare organization.
This “financial paperwork” is increasing operational costs and administrative burden on clinicians who can better spend their time on patients, their topmost priority. It might sound odd, but reports indicate that healthcare organizations can spend up to 14% of their revenue on billing and collection activities.
Robotic process automation and artificial intelligence services in healthcare are the logical solution for many providers in this case. Much like other industries, they automate important but repetitive functions like billing and claim processing.
In this blog, we’ll look at this healthcare workflow automation technique for medical billing and claim management, and how it benefits healthcare organizations.
Why is medical billing so hard?
You might be thinking that medical billing should be like hotel billing. But regular billing involves a buyer and seller or a service provider and client. That is not the case with medical billing in the US, where a few other factors are involved.

In the US, there are usually patients, providers, and insurance companies. According to the United States Census Bureau, 92% of people in the country had medical insurance at some point in 2022. The country has a network of government-sponsored and private healthcare insurance companies, such as Medicare, Medicaid, and private insurers.
So, providers rarely charge patients the full amount upfront; rather, they bill their insurers, which is called a claim. A claim is a formal request for payment that a healthcare provider sends to an insurance company after providing medical services.
Claim management
Now here, things get complex because every insurer has different rules and documentation. Therefore, medical professionals need to prepare and send claims to insurance companies, make sure the information is correct, and track what happens to each claim.
They also work with insurance companies to confirm what is covered, fix any errors, and solve payment issues. On the patient side, they may answer questions about bills, explain what insurance did or didn’t pay, and help patients understand what they owe.

This is a full-time job. No, seriously, a medical biller is a healthcare professional who manages the financial side of patient care. With the help of RPA and AI in healthcare, they can streamline insurance claims and patient billing to ensure providers get paid accurately and efficiently.
Medical coding
Medical codes are standardized labels that turn what happened in a healthcare visit into a format insurance companies can understand and pay for. It is like a common language between doctors, hospitals, and insurance companies.
For example, regular adult teeth cleaning has the code D1110 — Prophylaxis in the United States. There are several types of medical codes used in the healthcare industry, such as:
- ICD (International Classification of Diseases): ICD codes are created by the World Health Organization (WHO) and are used by many countries to classify diseases and health conditions.
- CPT (Current Procedural Terminology): CPT codes are used mainly in the United States for describing medical procedures and services.
- HCPCS (Healthcare Common Procedure Coding System): HCPCS codes are also US-based for billing Medicare and Medicaid patients.
Medical coding is done by reviewing medical records, identifying key information, and then selecting the right medical codes. Errors in medical coding can lead to claim denials. And before you ask, no, medical coding isn’t done like regular coding. A medical coder mainly works with electronic health records (EHRs) and billing systems.
Are you starting to see why robotic process automation in healthcare for medical billing makes sense? It is a complex process where you don’t just note down the price of acquired services and sum them up. Automating healthcare processes and creating intelligent workflows like is really important to change healthcare for the better.
What is robotic process automation?
RPA is a bit of a misnomer because there are no actual robots involved in it. It is an automation technique that uses software “bots” to perform repetitive, document-heavy tasks, such as:
- Data extraction
- Filling forms
- Generating reports
- Sending emails
These are the kind of repeatable, rule-based tasks that take up a lot of time of human workers.

RPA vs AI
Many people think of RPA as a form of AI, but they are distinctly different. RPA follows explicit rules defined by an end user. It does not make probabilistic decisions on its own. But some AI technologies have the capacity to understand, interpret, and make judgments on their own.
| RPA | AI |
| Follows a fixed set of steps like a checklist | Learns from examples and can handle new situations |
| Needs clean, predictable data | Can work with messy or varied data |
| Uses clear rules: “If X happens, do Y” | Uses patterns and probability to guess the best answer |
| Doesn’t really “think” and just does what it’s told | Can interpret and decide based on context |
| Requires reprograming to adjust changes | Can improve itself when trained with more data |
In other words, AI mimics human intelligence, while RPA replicates human-directed tasks. However, both are complementary technologies that are often used together as part of intelligent automation.
Improving medical billing through robotic process automation in healthcare
There is an urgent need for healthcare workflow automation. The industry is facing the dual challenge of staffing shortages and increasing workloads almost everywhere.
RPA use cases in healthcare are many, but robotic process automation in healthcare works best with repetitive, rule-based paperwork like medical billing and claim management. Medical billing professionals can use it to shift from their current reactive approach to a proactive one.
1. Accurate patient registration
It is not uncommon for things to go wrong before the patient even sees a doctor. Normally, patient registration requires collecting details like the patient’s prior records and insurance details. All of that needs to be copied from one screen to another. And if a mistake happens here, it will cascade through the entire billing process.

Robotic process automation in healthcare can do this boring part faster and better than humans. RPA bots can extract the patient information automatically from various sources and enter that data precisely into the target system. And if the bot finds missing or inconsistent data, it flags the case for a human to review.
2. Faster insurance verification
Health insurance can be tricky. Employers may change healthcare plans without notice, premiums may increase, or the patient may switch their insurer. Therefore, a provider needs to confirm that the patient’s insurance is active, current, and will cover the services being provided.
Traditionally, staff often have to contact insurance companies, log into multiple payer portals or databases, and sometimes follow up multiple times to confirm coverage details. But with robotic process automation in healthcare, bots can quickly pull patient details from different systems, check coverage through payer portals, and confirm eligibility in real time.
Faster verification also means patients get quicker answers about what their insurance covers, which makes life easier for them as well.
3. Improved claim management
Robotic process automation in healthcare can massively improve the claim creation and submission process. RPA bots do not get bored while trying to sort out the minutiae of medical coding. This makes them good at tedious precision.
A trained RPA bot can create an accurate claim from A to Z with pinpoint accuracy. And all of that matters because the faster a claim gets out the door, the faster the provider gets paid. It reduces the gap between care delivered and money received, which is what keeps the lights on.
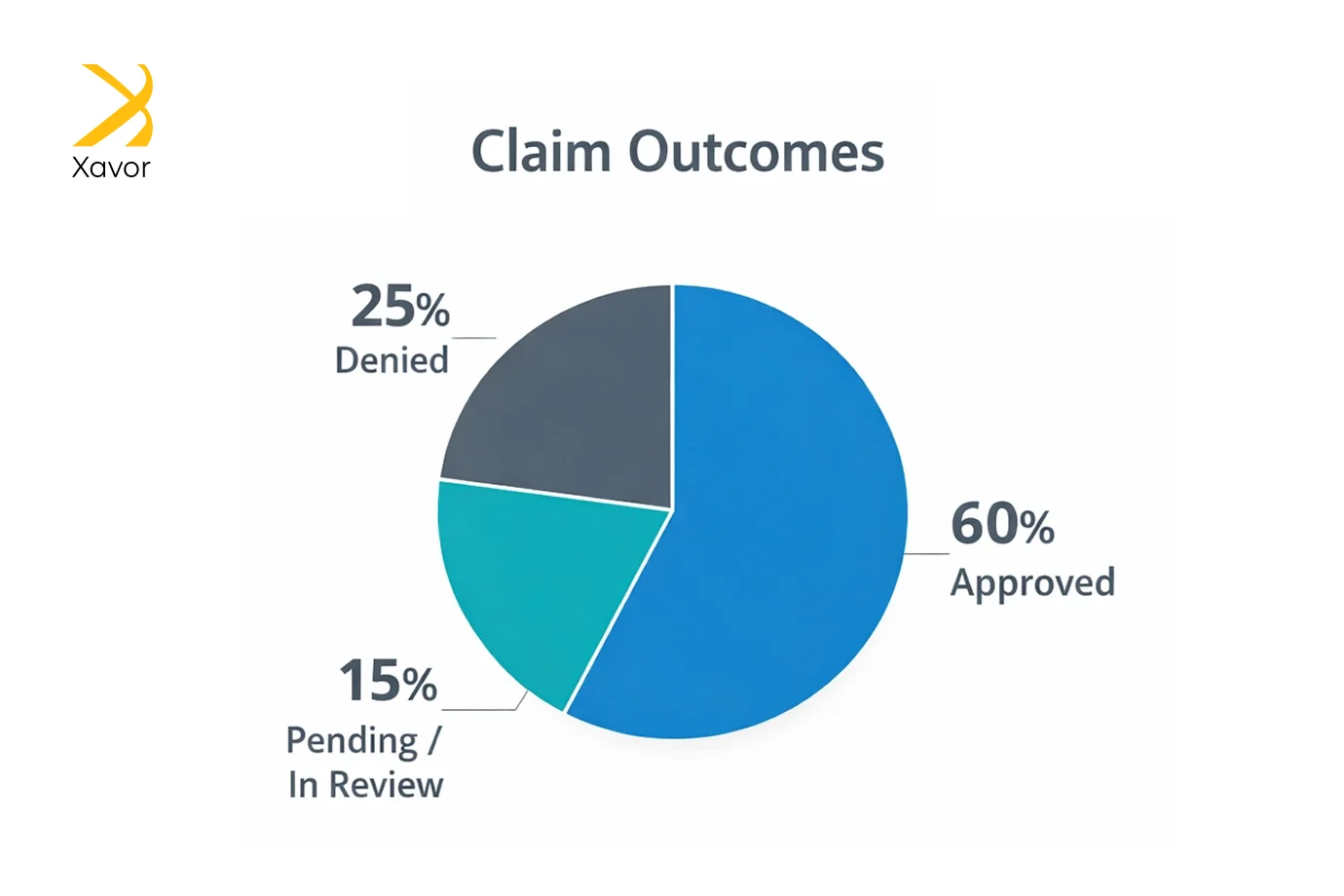
Furthermore, submitting a claim is not the end of the story. Claims can get approved, rejected, or stuck in limbo forever. That is why someone has to keep checking. But it’s a lot of work.
RPA can automate this too by:
- Checking claim status across multiple payer portals
- Identifying claims that need attention
- Sorting them by what action is needed
4. Better denial management and appeals
American healthcare insurance companies can have claim denial rates of 20–30%. Sometimes the “no” is reasonable. Sometimes it’s because someone typed one digit wrong. Either way, the provider doesn’t get paid until the denial is fixed.
You can use robotic process automation in healthcare to handle denials and make resubmissions. If a claim was rejected because of something minor, the bot can correct it and resubmit it immediately. That “immediate response” is a big deal because it keeps claims from sitting in limbo for weeks. And limbo is expensive.
For complex denials, the ones that require medical judgment, it can refer to human judgment.
And sometimes an insurance company denies a claim, and the provider believes it should be paid, so they can appeal that decision. Robotic process automation in healthcare can help here, too.
For appeals that follow standard patterns, RPA bots can:
- Generate appeal letters using templates
- Fill in patient- and claim-specific details automatically
- Attach the right supporting documents
- Submit everything within the required timeframes
Conclusion
The administrative side of healthcare is an industry of its own. Unfortunately, people seem to have accepted the chaos of medical billing as normal. But with robotic process automation in healthcare, even the most error-prone, repetitive parts of healthcare can be improved by leaps and bounds.
Every hour clinicians spend rechecking eligibility, rekeying data, or chasing claim statuses is an hour that healthcare organizations are paying for work that doesn’t improve care. Automating healthcare processes like medical billing and claim management protects time, attention, and energy to focus on what genuinely requires judgment and human expertise.
RPA use cases are one of the fastest ways to start building that kind of organization. It’s practical, scalable, and designed for the messy reality of healthcare workflows.
Partner with Xavor to automate your revenue cycle with purpose-built RPA solutions. We have helped Fortune 500 healthcare organizations design, deploy, and scale automation without disrupting their operations.
Contact us at [email protected] to book a free consultation session.
FAQs
Robotic Process Automation (RPA) in medical billing uses software bots to handle repetitive billing tasks like patient data entry, insurance verification, claim creation, and claim status checks. It helps reduce errors, speed up reimbursements, and frees staff to focus on complex cases and patient support.
The three types of RPA are attended RPA, where bots support staff in real time while they work. Unattended RPA, where bots run fully automated tasks in the background without human involvement; and hybrid RPA, which combines both approaches to automate end-to-end workflows efficiently.
The 4 D’s of automation are Dull, Dirty, Dangerous, and Dear. It is a way to describe the kinds of tasks automation is best suited for. In simple terms, automation works well for work that is repetitive and boring, messy or unpleasant, risky for people, or costly and time-consuming to do manually.

